Experts are cautiously concerned, but this is a fundamentally different outbreak.
On Wednesday, the CDC confirmed a case of monkeypox in a Massachusetts man who had recently traveled to Canada.
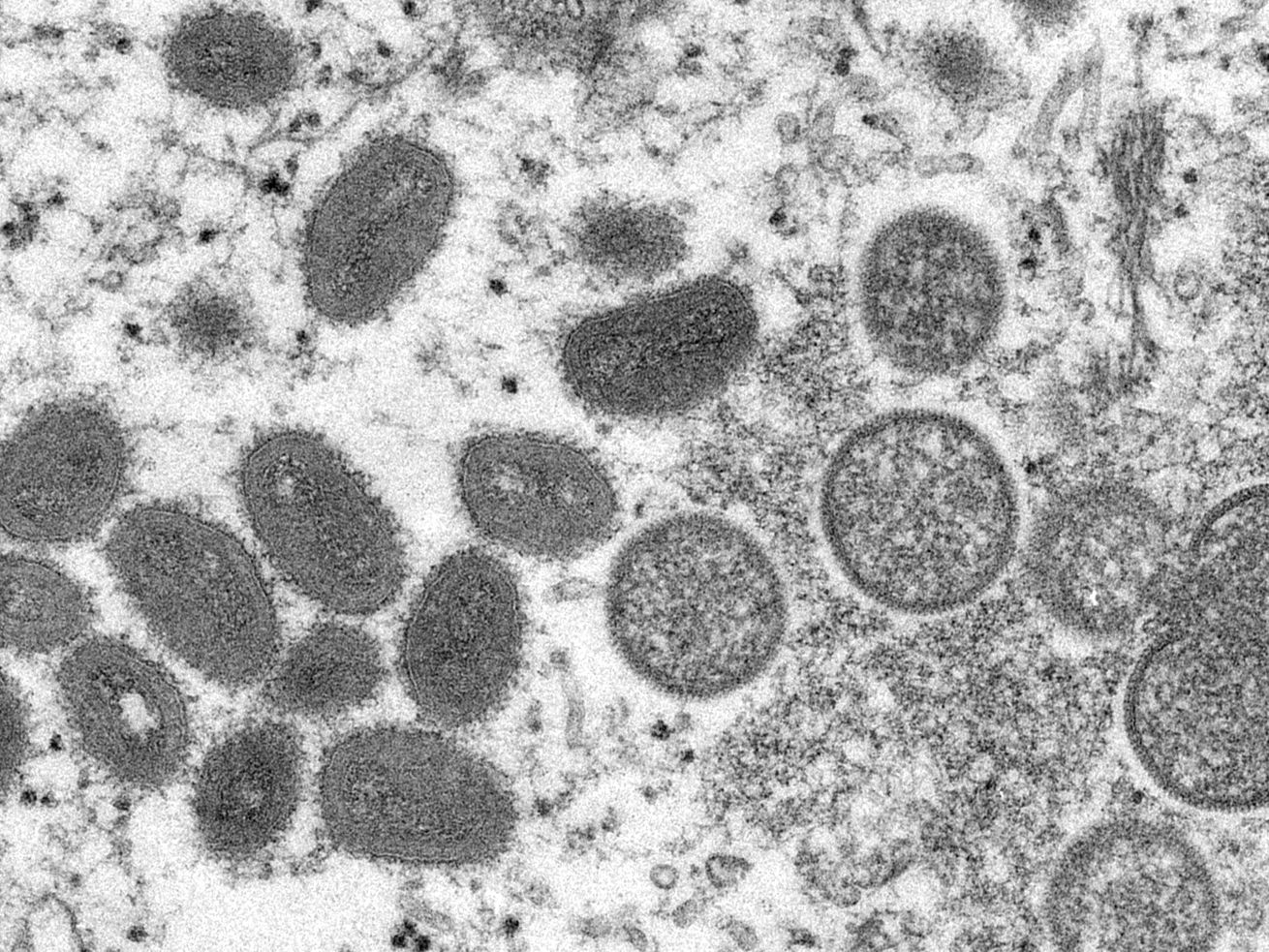
It wasn’t the first time the US has seen a case of monkeypox, a virus related to smallpox that causes flu-like symptoms and a rash, and can sometimes be deadly. Occasionally, public health authorities identify single cases in people recently returned from West or Central Africa, where the disease is more common.
What’s different — and concerning — about this Massachusetts case is that it’s occurring as clusters of monkeypox infections are popping up in other countries where the virus is also rare.
Since early May, the UK Health Security Agency has detected a total of 9 cases of the infection, and Portugal and Spain have reported 14 and 23 suspected cases, respectively. (The numbers are changing rapidly; a University of Oxford epidemiologist tweeted a link to a makeshift tracker where you can see the latest figures.)
With so many monkeypox cases concurrently popping up in different countries, public health officials’ immediate questions are whether the cases are related, and whether monkeypox is spreading in other communities undetected.
“The worldwide concern from public health authorities is trying to understand how these are related to each other and what the causes are,” said Agam Rao, an infectious disease specialist and poxvirus expert at the CDC.
Only weeks into this outbreak, it’s too early to tell what exactly is going on, and whether this outbreak has epidemic potential. For the time being, said Rao, the general public doesn’t need to be particularly worried. “The risk is still very rare,” she said, and the strain of monkeypox currently being detected is relatively mild.
Two years into a deeply divisive global pandemic, word of another pathogen spreading unchecked might make some people want to launch themselves directly into the sun.
But with monkeypox, the world faces a very different situation than in the early days of Covid-19. Monkeypox, unlike SARS-CoV-2, is a known quantity. We have more tools to prevent and treat it — far more than we did for Covid-19 at the outset of the pandemic — and both public health and the general public have had a lot of practice taking measures to prevent infections from spreading. Still, the trajectory of the outbreak is as yet uncertain, and public health experts remain vigilant.
What is monkeypox?
Monkeypox viruses generally circulate among wild animals in Central and West Africa, and usually spread to people when they eat or have other close contact with infected animals. The virus was first identified among research animals at the CDC in the 1950s (that’s how it got its name “monkeypox”), and for a long time afterward, human infections were sporadic, even in countries where lots of animals are infected.
That’s partly because monkeypox is related to the smallpox virus, and immunity to smallpox is protective against monkeypox. But as of 1980, smallpox has been eradicated in humans, and vaccinations against smallpox have grown rare — and human cases of monkeypox have been on the rise. It’s still rare: According to the CDC, Nigeria has reported 450 cases since 2017, when public health authorities began seeing more cases among humans.
Infection with the monkeypox virus usually causes a flu-like illness with fever, headache, muscle aches, swollen lymph nodes, and a rash. Although monkeypox is not related to chickenpox, the characteristic monkeypox rash looks a lot like it, starting as red spots on the mouth and face, then spreading to the arms and legs. Over four to five days, the spots turn into small fluid-filled blisters that are often tender to the touch, eventually become doughnut-shaped, and begin to crust over by the two-week mark.
/cdn.vox-cdn.com/uploads/chorus_asset/file/23575738/GettyImages_909695428t.jpg) Smith Collection/Gado via Getty Images
Smith Collection/Gado via Getty Images
Studies have suggested the virus’s R0 — the number of people who will hypothetically contract a communicable disease from a person infected with that disease — is relatively low, somewhere between one and two.
“It’s not as highly transmissible as something like smallpox, or measles, or certainly not Covid,” said Anne Rimoin, an infectious disease epidemiologist at the University of California Los Angeles with expertise in monkeypox and other emerging diseases.
Transmission can occur through close contact with body fluids of an infected person, sores, or items that have touched fluids or sores (like bedding); the virus can also spread via respiratory droplets or aerosols that linger in the air. But unlike Covid-19, where people who are infected can spread the disease before getting sick, monkeypox isn’t considered contagious before people develop symptoms.
There are two predominant strains of monkeypox: the “West African” version and the “Congo Basin” version. Of the two, the Congo Basin version has historically spread more easily from person-to-person and caused more deaths. The current outbreak involves the West African version.
The infection does not commonly lead to deaths in high-resource countries like the United States because people living there generally have better access to the supportive care that resolves most monkeypox infections, said Rimoin. In 2003, at least 53 people in the midwestern United States caught the infection from pet prairie dogs who’d been infected when they were housed near rodents imported from Ghana; none of the infected people died.
In rural parts of Africa, where access to hospital care is lower, infection has led to death in about 4 percent of people infected with the virus.
Several treatments approved for smallpox treatment could potentially be used to treat monkeypox infections if necessary. However, most cases are relatively mild; it’s unclear whether any of the currently affected patients needed or received any of these medications.
What’s different about the latest monkeypox cases?
The latest clusters of monkeypox cases are different from previous clusters in a few ways.
For starters, the current cluster involves many infections happening concurrently beyond the African countries where the disease circulates in wild animals. “We’ve never had a situation where so many cases have occurred outside of those countries concurrently,” said Rao.
What’s also unusual about the latest cases is that many of them so far have occurred among men who have sex with men (monkeypox transmission has not previously been associated with sexual preference or intimate contact). Many of the cases are presenting with clusters of pimple-like spots in the genital area — an uncommon area for the monkeypox rash to start.
After clinicians made the first few diagnoses among men coming to sexual health clinics with unusual rashes, health officials began asking sexual health clinics to look out for monkeypox cases. This doesn’t mean monkeypox is only circulating among men who have sex with men, and some infections have been diagnosed in people who are not gay or bisexual men.
“We’re finding where we’re looking,” Maria Van Kerkhove, a World Health Organization emerging diseases and zoonoses expert, said in an interview with STAT.
If this monkeypox outbreak does end up linked to sexual networks among men, that doesn’t mean it’s necessarily a sexually transmitted infection; it may simply be a question of who’s getting close enough to an infected person to get infected, themselves. Other germs spread by close — but not specifically sexual — contact have previously caused clusters of infections among gay and bisexual men and college-aged students, such as meningitis, a disease spread by respiratory droplets in close settings.
How concerned should the general public be about this outbreak?
In addition to trying to understand the cause of the current outbreak and the routes of transmission, public health authorities are working to sequence the viruses isolated from individual patients to better understand whether it has changed in any ways that might make it more or differently transmissible, said Rao.
For the moment, however, there’s no reason to think the virus has undergone any meaningful mutation, she said.
Currently, the general public doesn’t need to be particularly worried about the risk monkeypox viruses pose to themselves and their loved ones. “It does not spread easily from person to person, the risk to the general public is low,” said Rimoin. And with health providers now on high alert for the infection, it is more likely to be recognized quickly among people who do get infected and quickly contained, halting chains of transmission.
“We’d have to see a significant cluster of cases events and ongoing transmission” before public health authorities put any broad preventive measures in place, said Rimoin.
Even a large monkeypox outbreak would likely be much easier to handle than the Covid-19 pandemic. For one, the fact the virus isn’t considered contagious before people show symptoms could make it harder for people to unknowingly spread it. And in addition to treatments, we already have excellent vaccines to protect those at highest risk from infection — public health authorities in the UK are currently vaccinating close contacts of cases to prevent further spread of infection.
This isn’t a novel disease — so if monkeypox does become a much larger outbreak than it already is, public health authorities are better equipped with tools to manage it.
In fact, as a consequence of the Covid-19 pandemic, public health is in a relatively strong place to handle this outbreak.
“I think we’re in a good position to respond to monkeypox because most health departments have staffing, lab networks, and funding from Covid that can be used for emergency response,” said Jay Varma, a physician and epidemiologist based in New York City who recently was senior advisor to the Africa Centers for Disease Control and Prevention. “The real risk is what happens when that funding runs out over the next few years.”
0 Comments